PART FOUR: CREDIT WHERE CREDIT IS DUE
This is the fourth of an eight-part patient advocacy manifesto, I Dissent.
This is the fourth of an eight-part patient advocacy manifesto, I Dissent.
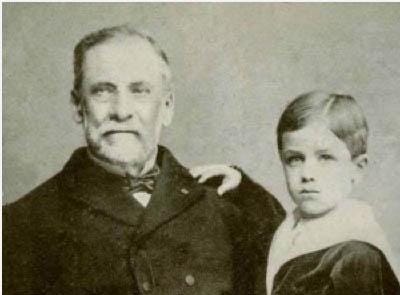
From The Pasteur Institute: Louis Pasteur with Joseph Meister, the first human to receive Pasteur's rabies vaccination.
“Those who came before us made certain that this country rode the first waves of the industrial revolutions, the first waves of modern invention, and the first wave of nuclear power, and this generation does not intend to founder in the backwash of the coming age of space. We mean to be a part of it – we mean to lead it.” ~ JFK
ON THE SHOULDERS OF GIANTS
So far, I have been critical – so let’s take a step back and acknowledge greatness. In the last 150 years, the advent of pharmaceuticals and vaccines has transformed human existence. Life expectancy has soared, and, notwithstanding the current COVID-19 pandemic, dying of infection has become a thing of the past. Now, we die of inflammation.
In 1885, Louis Pasteur’s discovery of the rabies vaccine kicked off a field of study that would lead to the eradication of infection as the leading cause of disease and greatly extend lifespan. This milestone in pharmacology began when Joseph, a nine-year-old boy who was attacked by a rabid dog, was the first person ever to receive the rabies vaccine that Louis Pasteur developed.
While developing the vaccine, Pasteur theorized that if a person or animal were exposed to a weakened version of the virus, their body would develop the natural mechanisms necessary to fight it. When Joseph was bitten, he was brought to the scientist, who met with his colleagues to discuss the ethics of treating young Joseph: if they didn’t, he would surely die, or they could try, and it could save his life.
On July 6, 1885, Joseph Meister became the first human vaccinated for rabies. He grew up to become the caretaker of the Pasteur Institute.
Pasteur’s invention of the rabies vaccine led to his coining of the ‘Germ Theory of Disease,’ which stated that germs are the central cause of disease. Germ Theory replaced Claudis Galenus’ ‘Humoral Theory of Disease,’ which was the predominant belief for 1500 years prior, which stated that four humors, or fluids, were the cause of disease – either black bile, yellow bile, phlegm, or blood, and that an imbalance of those humors caused disease.
The development of vaccines has led to a major decline and the prevention of infectious diseases, including whooping cough, tuberculosis, tetanus, rabies, typhoid fever, anthrax, cholera, yellow fever, typhus, influenza, polio, the measles, mumps, rubella, chickenpox, pneumonia, meningitis, hepatitis B and A, and more.
The World Health Organization has stated that vaccinations save 2 to 3 million lives per year. Improved access could save another 1.5 million.
Unfortunately, society has developed a short memory, and vaccinated adults choose to not vaccinate their children, and now we watch as diseases that were eradicated now making a comeback. The measles has increased by 30%. From 2001 to 2015, the number of babies and toddlers not vaccinated has quadrupled.
Many of us need to search no further than a couple of generations back to see what our ancestors suffered and died of that we don’t need to suffer or die from today. My great uncle died of the Hong Kong Flu in the 60s, and his brother, my other great uncle, suffered from lifelong cognitive impairment due to having the measles as a child. My great aunt spent a year living in an iron lung in NYC when she was a child and struggled physically for her entire life from the impact of Polio.
Following this era of exceptionalism with the advent of vaccines, the age of the antibiotic dawned – ‘antibiotic’ translating to ‘against life,’ as the Greek for life is the word bios, and obviously, the prefix ‘anti’ meaning opposed to.
In 1928, Alexander Fleming’s discovery and development of penicillin provided effective treatment for dangerous and sometimes fatal infections.
Later, Howard Florey, Ernst Chain, and their colleagues translated penicillin from bench to bedside. Stagnated by World War II and unable to garner high production of penicillin, the British pharmaceutical companies Glaxo (now GlaxoSmithKline, an early investor in bioelectronics) and Kemball Bishop (later bought by Pfizer), stepped up to the plate. Soon, penicillin production was brought to the United States, thanks to funding from the Rockefeller Foundation – always a key player in transformative medical research, including bioelectronic medicine.
Fleming’s discovery heralded a new age that led to the development of antibacterials, antivirals, anti-fungals, and anti-parasitics, with some designed as broad-spectrum to fight many organisms, and narrow spectrum, which is more targeted.
The age of antibiotics finally provided tools for doctors to treat their patients who came down with dangerous infections caused by rheumatic fever, meningitis, strep throat, tuberculosis, and even infections from cuts and scratches.
Much like Pasteur, Fleming completely transformed the paradigm of healthcare.
Of course, now we live in a time where superbugs are at risk of society developing antibiotic resistance due to over-using antibiotics for minor colds that would naturally work themselves out, because we don’t want to deal with the sniffles, but are apparently tough enough to watch children and the immunosuppressed die or face permanent impairment from diseases we once eradicated.
Outside of the realm of infection, Sir Frederick Banting, Charles H Best, and JJR Macleod’s collaboration to develop insulin in 1921 turned diabetes from a once fatal disease to a treatable, chronic disease. Following the addition of collaborator James Collip, a biochemist who purified insulin for safety in humans, fourteen-year-old Leonard Thomas was the first to have his unmanageable type 1 diabetes treated in January of 1922.
(As the daughter of a dad who has battled type 1 diabetes for 48 years, I am especially grateful for this.)
Julia Belluz reports in Vox, “When inventor Frederick Banting discovered insulin in 1923, he refused to put his name on the patent. He felt it was unethical for a doctor to profit from a discovery that would save lives. Banting’s co-inventors, James Collip and Charles Best, sold the insulin patent to the University of Toronto for a mere $1. They wanted everyone who needed their medication to be able to afford it.”
Among the many great discoveries of transfusion medicine, in 1916, Francis Rous and J.R.Turner figured out that adding 2% sodium citrate to blood could allow for the storage of blood for life-saving procedures.
William T.G. Morton was the first to anesthetize a patient for surgery, calling his drug ‘Letheon,’ “named after the Lethe River of Greek mythology, noted for its waters that helped erase ‘painful memories.’” Morton’s discovery led to the advances in general anesthesia today, whereas alcohol and opium – and literally ‘biting a bullet’ – were used prior.
As we can see, advances in pharmacology over the last 150 years have completely transformed not only how long humans live but also improved how we experience existence itself.
And all of this brings us to today, where we are now at the precipice of the next great revolution in medicine that stands to further advance the human experience in both quality and length.
Following Pasteur’s Germ Theory of Disease, which guided medicine for more than a century, Dr. Kevin Tracey’s discovery of the Inflammatory Reflex led to his coining of a new theory: the Cytokine Theory of Disease.
While infection (germs) can play a role in causing disease, it is inflammation – cytokines – that cause the damage associated with disease. It is not necessarily infection that causes lethality – it is the person’s own immune system overproducing inflammation.
What is revolutionary about bioelectronic medicine is that it dismantles the paradigm that the only way to treat and cure disease is through pharmaceuticals.
Homeostasis is a result of the nervous and immune systems communicating properly, using neural mechanisms. To achieve homeostasis, the body needs to have the perfect balance of inflammatory cytokines and anti-inflammatory cytokines.
In a healthy person, the body uses neural mechanisms to deliver neural signals back and forth between the immune system and the brain to maintain homeostasis – or in the event of upset due to illness or injury, uses that communication to determine the level of response.
For those with inflammatory diseases, this mechanism is faulty and malfunctioning. Using electrons rather than molecules, bioelectronic medicine seeks to control and reset the body’s natural rhythm.
Pharmaceuticals have played a pivotal role in the eradication of diseases of yesterday such as polio, measles, and more; insulin has saved the lives of millions of diabetics; antibiotics have made dying of infection the exception and not the rule. A debt of gratitude is owed to our Historical Giants who sought great discoveries, not for the sake of profit, but solely for the cause of eradicating a form of human suffering.
As time goes on, it will be necessary that researchers produce new drugs to address acute issues that will arise, like superbugs due to antibiotic resistance, and vaccines for viruses that can become pandemics, as we are witnessing today. Luckily, we have the privilege of the advances in research that led to the quick turnaround of revolutionary mRNA vaccines.
While pharmaceuticals have played their part in advancing medicine and extending life expectancy, the story of how we can continue to do that does not end there – and bioelectronic medicine proves that.
In his Ted Talk, world-renowned physician-scientist Siddhartha Murkhegee said, “When an architect builds a model, he or she is trying to show you the world in miniature. But when a scientist builds you a model, he or she is trying to show you the world in metaphor. He or she is trying to create a new way of seeing. The former is a scale shift, the latter is a perceptual shift. Antibiotics created such a perceptual shift in our way of thinking about medicine that it really colored, and distorted, very successfully, the way we thought about medicine for the last 100 years. But we need new models to think about medicine in the future — that’s what’s at stake. There’s a popular trope out there that the reason we haven’t had a transformative impact on the treatment of illness is because we don’t have powerful enough drugs, and that’s partly true. But perhaps the real reason is that we don’t have powerful enough ways of thinking about medicines. It’s certainly true that it would be lovely to have new medicines but perhaps what’s really at stake are three more intangible M’s: mechanisms, models, metaphors.”
THE AD AUCTION
Revisiting the aforementioned statement that patient foundations and pharmaceutical companies are benefitting from this cultural self-imposed totalitarianism per identity, they have profited in their quid pro quo partnership: the patient foundation promises patients that they are ‘committed to the cure’ while their funding comes from sponsorships of large pharmaceutical companies who manufacture expensive and often ineffective immunosuppressive drugs that have resulted in a bloated anti-inflammatory market worth a staggering $100 billion dollars.
Johns Hopkins Bloomberg School of Public Health and West Health Policy Center found that Big Pharma would still be “the most profitable industry sector” even if it lost $1 trillion in sales.
The argument from patient foundations as well as patient advocates who defend the interests of Big Pharma state that these companies need massive profits for research and development. Unfortunately, many of those companies spend around $56 billion more on stock buybacks than they do on research – and the beneficiaries of those buybacks are executives who are given thousands of shares of stocks on top of millions in compensation. Meanwhile, in 2020, drug makers spent $314 million lobbying Congress.
Meanwhile, according to the Rand Corporation, “nearly 60% of Americans have at least one chronic condition, 42% have more than one, and 12% of adults had five or more chronic conditions.” Worldwide, chronic inflammatory diseases kill three out of every five people.
Never one to miss an opportunity for an easy sale, this is a perfect audience for TV ad execs to market expensive pharmaceutical commercials.
For every dollar that large pharmaceutical companies spend on research and development, they spend nineteen dollars on marketing through direct-to-consumer commercials in both America and New Zealand. From 2015 to 2018, the pharmaceutical giant Abbvie spent $1.5 billion on Humira commercials, and what’s more, drug advertisements are a tax write-off for pharmaceutical companies – so it didn’t actually cost them a dime.
Efforts to regulate – let alone ban – pharmaceutical commercials have been met by the PhRMA lobby’s lawyers arguing that to do so is a violation of pharmaceutical corporations’ first amendment rights. This, of course, comes from the same lobbying firm that released their own ad on behalf of their members in industry, stating a false and misleading claim that regulating the cost of prescriptions would negatively impact the research and development of future treatments and cures.
Ironic, indeed, coming from industry lobbyists who know full well how much industry is spending on pharmaceutical ads to target patients who they view as consumers – the problem with doing so, however, is that to view a patient as a ‘consumer’ suggests that medication is a product to be consumed, not a remedy to treat an ailment, and therefore, a profit to grow.
According to Medical Marketing & Media magazine, pharmaceutical marketers spent $5.1 billion on TV ads in 2018 alone, with Pfizer adding $1.1 billion to the pot – including $209 million on Chantix for smoking cessation and $158 million on rheumatoid arthritis and ulcerative colitis drug Xeljanz, which, in 2021 was slapped with a black box warning by the FDA due to the drug having higher risks of serious adverse events such as heart attack, stroke, and blood clots — even at lower doses.
That same year, “Eli Lilly spent $517 million, including $243 million promoting its diabetes treatment Trulicity. AbbVie, Amgen, and AstraZeneca rounded out the top five pharma spenders,” according to Nielson, powerhouse leader of evaluating audience insights.
With 8% of TV networks’ ad revenue coming from pharmaceutical commercials, in a corporatized world that measures profit over duty, Kantar’s ad insights show that CBS banked $1 billion in pharma ad revenue from November 2017 to December 2018, and then ABC at $641 million, and NBC at $593 million.
Disturbingly, it’s no longer your mother’s direct-to-consumer advertising moving forward, according to ad exec Flora McKiernan. ABC pioneered a new approach: selling episodes of popular sitcoms to the highest bidder, with the show Black-ish writing an episode around one character’s new diagnosis of diabetes. Without mentioning sponsor Novo Nordisk by name in the episode, it was paired with ads during commercial breaks for Novo’s products, which include Ozempic, Rybelsus, and Victoza.
The next morning, the dialogue continued for a segment on Good Morning America.
Steve Barrett writes, “McKiernan says every other pharma company came calling after the activation and asked how they could get in on the action.”
Later in his article, Barrett writes of how ad-sale execs get “twitchy” when brand-name drugs age and generics become available. “There were a lot of nervous people when Cialis and Viagra went off-patent, but there are enough drugs in the pipeline,” says Ross. “If you watch us on any given night, you’ll see drugs for high blood pressure, psoriasis, rheumatoid arthritis, smoking cessation — the whole gamut. I’m optimistic about continued increased spending in 2019.”
While generics may make CBS president and chief advertising revenue officer Jo Ann Ross twitchy, patients may find themselves twitchy over her use of the word optimistic.
So, is there a market for the cure to co-exist in the profitable world of disease?
“Part Five: Metal Concerts for Migraines” coming tomorrow.