PART THREE: THE STAKES
This is the third of an eight-part patient advocacy manifesto, I Dissent.
This is the third of an eight-part patient advocacy manifesto, I Dissent.
Representation of Galileo Galilei displaying his telescope in Venice. Author: H. J. Detouche
“The exploration of space will go ahead, whether we join in it or not, and it is one of the great adventures of all time, and no nation which expects to be the leader of other nations can expect to stay behind in the race for space.” ~ JFK
FIRST, DO NO HARM.
It’s been said that the most dangerous sentence in the English language is, “But we’ve always done it this way.”
Medicine is often practiced in a very dogmatic way, in that when a certain style of treatment – in this case, immunosuppression – is the only treatment available for so many years, the medical community begins to think it’s the only way to treat disease. With so many biologics and DMARDs in the arsenal to pull from, there’s always a new one to try, and when new therapies come on the market touting a slightly different cytokine target or subunit, it’s welcomed and celebrated as a ‘win’ for drug-refractory patients.
After all, physicians should be looking for new therapies for patients; they see how desperately those therapies are needed. In a newly published paper on net remission rates of patients on biologics after approximately one year, the results are dismal:
Remicade: 16.7% at 54 weeks
Humira: 17.4% at 56 weeks (28.6% TNF-naïve)
Entyvio: 6.7% at 56 weeks (18.7% TNF-naïve)
Stelara: 13.9% at 44 weeks (39.8% TNF-naïve)
For Crohn’s patients, this isn’t even endoscopic remission, which is usually significantly lower.
Nonetheless, dogma dictates the dialogue of the day. When novel therapies or practice modalities become available, physicians are skeptical, criticizing them regardless of data collected by randomized trials. Eventually, after decades, they reluctantly submit to utilizing it. After that, the fascinating phenomenon of confabulation occurs, and it is then misremembered as either their idea — or, they were early, ardent pioneers of it.
Or, others in the field try to inflate their role in its early days while attempting to deflate the larger roles of others, and then attempt to rewrite history to their benefit.
Regardless of how the destination is reached, however, the Hippocratic Oath should remain at the forefront of decision making and care, which shouldn’t be hindered by the haughtiness of veterans dismissing discovery backed up by rigorous data as “ineffective” or not as thorough as the current standard of care, and then hemming and hawing over toeing the line for hospital reimbursements, or the frustration of now having to deal with continuing medical education and staff training — as has been shown in recent months while Dr. Michael Todd Dolinger of Mount Sinai, a pioneer of using ultrasound to evaluate disease activity rather than more invasive methods, has often been met on #MedTwitter and #GITwitter with, first, “Well, it can’t be as thorough as colonoscopies,” and then followed by, “Well, even if it could be, how are we supposed to get properly reimbursed for this versus colonoscopies? And what about staff training? Now we have to buy an ultrasound machine too?”
While many have shown their excitement over this innovation, veterans in the field curmudgeonly scoffed, first at the evidence, and then at their perceived potential hiccups in its rollout.
While all new therapies and practices should be thoroughly evaluated and peer-reviewed, there is something to be said for the adoption of a fixed versus growth mindset.
BLACK BOX REALITIES
Recently, an acquaintance with Crohn’s was diagnosed with non-Hodgkin’s large B-cell lymphoma, which her doctors have said is a result of being on Remicade. What’s more, she discussed her need to find an alternative treatment other than immunosuppression for her Crohn’s because of the risk of the cancer returning.
While dealing with a new cancer diagnosis, she is also now, once again, up against a Crohn’s flare that has landed her back in the hospital, down forty pounds off her already petite frame, contemplating the need for surgery with her medical team, and back on the very drug that caused her to develop lymphoma.
This is just one example of how the status quo can, and does, upend the lives of everyday patients who are just trying to live as fully as possible.
For other patients, as the days pass and the treatment options available to them fail, some of them will lose their jobs and their livelihood due to their disease.
Some of them will see permanent physical damage that will be too late to reverse.
Many of them will develop new co-morbidities, as we all know that inflammatory diseases often travel in packs. Some will lose their homes while attempting to mortgage their hospitalizations and treatments. And some will die from complications due to inflammation, whether from sepsis, cardiovascular issues, or from cancers they develop as a result of the black-box treatment options they are on now, or they will develop cancers from the course of their disease progressing to the point of no return, metastasizing from an inflammatory, oxidative environment to a cancerous one.
The lifespan in both length and quality of those patients who will see benefit from future novel therapies deserve to know that all stakeholders, including patient advocates, are doing everything they possibly can to give them that chance.
When JFK delivered his famous speech, he mused over the great advances that have been made in the last 50,000 years in humanity’s recorded history condensed into half a century. While there has always been critics of progress and celebrators of the status quo as a staple in any field, now, the larger culture has joined in a collective willingness to accept limitations, prop up the peanut gallery, and muse that progress is too tiresome a task to take on.
In JFK’s famous speech, he addressed those critics, saying, “it is not surprising that some would have us stay where we are a little longer to rest, to wait. But [this] country of the United States was not built by those who waited and rested and wished to look behind them. This country was conquered by those who moved forward – and so will space.”
So, too, will our future be conquered by these advances in bioelectronic medicine that will allow millions of those currently suffering the opportunity to thrive, and those who are not yet with us to never have to endure the same great pains that we have. They’ll have new woes to address, undoubtedly, but those woes will not be crippling inflammation.
Mary Oliver said it so eloquently: “And that is just the point... how the world, moist and beautiful, calls to each of us to make a new and serious response. That’s the big question, the one the world throws at you every morning. ‘Here you are, alive. Would you like to make a comment?”
THE UNRELIABLE CRITIC
Many in the medical field, pharmaceutical industry, and patient foundations have been critical of bioelectronic medicine. Their critiques have included those who say that patients who have benefitted from it are “an extraordinary example of the placebo effect,” or researchers who have said things like, “though Dr. Tracey may say that molecules and targets don’t always work, they often do, even though that hasn’t been the case for you,” or from a pharmaceutical executive I once met who told me that if what I’m telling him about bioelectronic medicine is true, he is “screwed” – because he’ll be “out of a job.”
I wish I could say that these all have been isolated experiences, but they haven’t. Over the last five years, I’ve lost count of the number of people who have criticized the field, or, from one national patient foundation in particular, argued that current treatment options are good enough – so what do we need new treatment options for?
Mark Twain once wrote, “Whenever you find yourself on the side of the majority, it is time to pause and reflect.”
When we evaluate events in history that became milestones that accelerated human progress, before those advances were accepted, they were vehemently denied by those who stood to benefit from the status quo remaining – and when outright denial didn’t work to squash progress, they argued that the new discovery was ‘dangerous’ to the wellbeing of the collective.
When Galileo adapted spyglass to get a better view of the moon, planets, and Milky Way, his observations confirmed Copernican Theory – that is, our solar system is heliocentric, meaning it revolves around the sun. This conflicted with the teaching of the Roman Catholic Church. In 1633, Galileo arrived in Rome, where the Roman Inquisition charged him with heresy, sentencing him to house arrest until his death in 1642. In the year 1992, a total of 359 years after Galileo’s imprisonment, the Vatican recognized its mistake in condemning the man who Einstein referred to as “the father of modern science.”
Other examples include Hungarian doctor Ignaz Semmelweis, who, in 1846, attempted to understand why women in the physicians’ maternity clinic were dying of ‘childbed fever’ at significantly higher rates than in the midwives’ clinic. After evaluating and testing different hypotheses, he discovered that the physicians in the maternity clinic with the higher rate of fatality post-childbirth were delivering babies after doing autopsies, which the midwives were not conducting.
Semmelweis’s discovery happened prior to Louis Pasteur’s Germ Theory of Disease. To test his theory, he instructed his medical staff to wash their hands and clean their instruments with chlorine. Maternity deaths dropped significantly.
Rather than celebrate this discovery, other physicians were insulted by the suggestion that they were the cause of those prior deaths.
Semmelweis was eventually committed to a mental asylum by his peers, where he was beaten, and eventually died at the age of 47.
Today, he is considered a pioneer of the age of physician-scientists.
In his Ted Talk, Ethan Hawke says, “If history has taught us anything, [it’s that] the world is an extremely unreliable critic.”
Someday, we will look back on present times and those who are currently working to stagnate the progress of bioelectronic medicine, and once again, find this to be true.
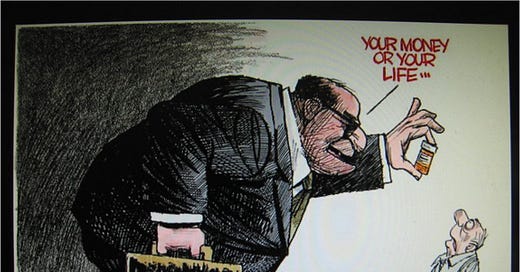
RACKETEERING
In clinical trials, drugs like Remicade, Humira, Enbrel, and other biologics only need 50% of the trial population to have a 20% reduction in symptoms for the FDA to consider these drugs ‘effective.’
Whenever a new TNF-inhibitor comes onto the scene, there is never pushback from patient influencers, patient foundations, or pharma – yet the mere suggestion of novel therapeutics to treat disease, such as bioelectronic medicine, is oft met with disdain and disregard – despite recently being given breakthrough device designation by the FDA, which states that vagus nerve stimulation clinical trials have shown greater efficacy than the current standard of care.
Meanwhile, the Department of Justice found that the maker of Humira, AbbVie Inc. – Janssen Biotech, Inc., a Johnson & Johnson subsidiary – has utilized an “anti-competitive scheme” that would maintain their monopoly by creating “pay-for-delay and market allocation agreements with biosimilar competitors,” as well as creating a “patent thicket” to prevent competition from biosimilars, “which would erode sales.”
What’s more, according to the House of Representative’s Investigation into Drug Pricing, the House found that AbbVie raised the cost of Humira “27 times, including by nearly 30% in one 10-month period” since 2003. Today, the cost of a 40-milligram syringe of Humira is now $2,984, or $77,586 annually — 470% more than when the drug was launched in 2003. The report also found that in 2020 alone, AbbVie collected “$16 billion in U.S. net revenue for Humira.”
What’s more, while AbbVie has been forced to reduce the price of Humira internationally, it has supplemented these losses by raising its cost for Americans.
Meanwhile, patent settlements with four biosimilar companies that would reduce cost through generics have cost the US healthcare system $19 billion.
In 2013, arthritis cost the US economy $304 billion dollars, and that same year, arthritis patients lost $252 million in wages from missing work due to their disease. Not to mention the 43% of patients who can’t afford their prescriptions, and the 9% that go without their drugs because of the cost.
The report goes on to say, “These price hikes contributed to billions of dollars in corporate profits and enriched company executives while harming American patients and taxpayers. AbbVie pursued a variety of tactics to increase drug sales while raising prices for Americans, including exploiting the patent system to extend its market monopoly, abusing orphan drug protections to further block competition, and engaging in anticompetitive pricing practices.”
If this is the extent that one drug company giant is willing to go to prevent access to more affordable biosimilars – to what extent will they go to preserve profits by preventing access to novel therapies that may allow patients... to no longer need biologics at all?
“Part Four: Credit Where Credit is Due” coming tomorrow.